The American Diabetes Association (ADA) has released its latest set of evidence-based clinical practice guidelines, the standards of medical care for people with diabetes. These guidelines are updated every five years and reflect the latest research and best practices. Hopefully, the changes will improve diabetes care for people living with the disease. Read on to learn more. Listed below are a few of the key changes. Listed below are the key points to remember about the new guidelines.
Table of Contents
ACOG gestational diabetes guidelines blood sugar readings
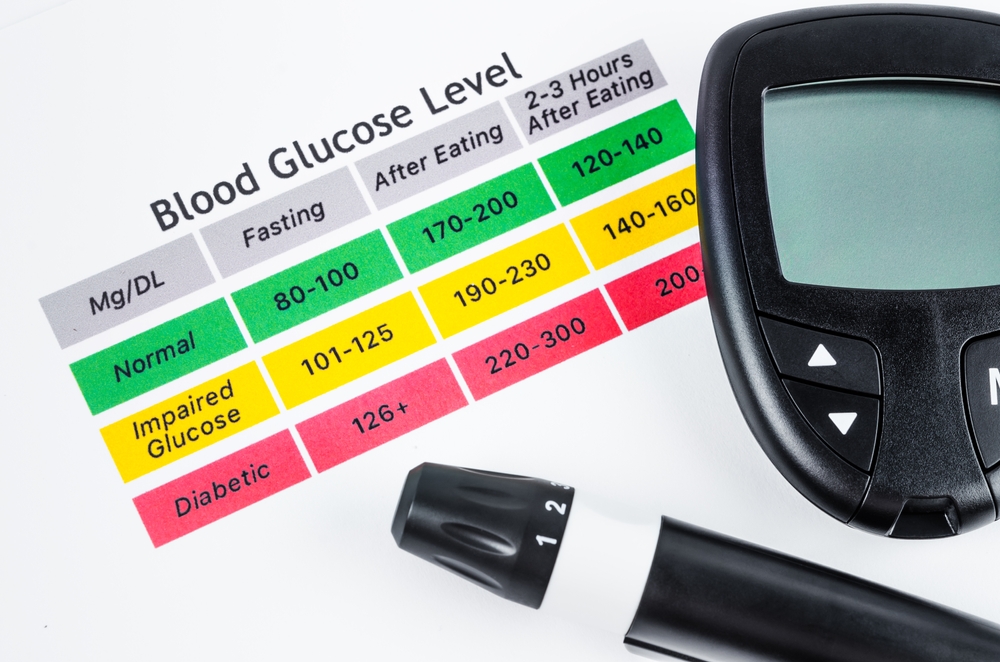
Accurate blood sugar readings are crucial during pregnancy. According to the ACOG guidelines, the glycemic target range is between 6.1 and 7.1 mmol/L, which is a range of around 4 to seven. In women who have poorly controlled diabetes, blood glucose levels are often at the level of 6.1 mmol/L or less. However, blood sugar levels over this range are associated with increased risk of neonatal hypoglycemia and birth asphyxia. Women with poorly controlled diabetes have an increased risk of developing disproportionate fat around the shoulders, which doubles the risk of shoulder dystocia.
The American Diabetes Association recently published the new standards for glucose tolerance testing, which differ from the recommendations of ACOG. However, the new guidelines call for a 75-gram glucose tolerance test performed at the first prenatal visit for women with risk factors for type 2 diabetes. The results of a screening test that shows high blood sugar levels will often require a second diagnostic test, according to the NIH.
Several factors contribute to the emergence of gestational diabetes, and the current blood glucose levels used to diagnose it can change over time. Some tests use lower cutoff levels than others, resulting in more women being diagnosed with GDM. The proposed International Association of Diabetes and Pregnancy Study Groups cutoff levels would classify 18 percent of pregnant women in the U.S. as having GDM.
The current guidelines for gestational diabetes are the most widely used. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) proposed new blood sugar cutoffs for diabetes in pregnant women in 2010. These guidelines have been adopted in many countries, although the U.S. has not embraced them. However, it is not too late to switch to the new blood sugar guidelines for gestational diabetes.
Screening

New guidelines for screening for diabetes released by the US Preventive Services Task Force and the American Diabetes Association recommend lowering the age at which overweight and obese individuals should first undergo a blood glucose test. This change will help increase the number of people who receive the recommended annual screenings for the condition. By lowering the age, this new policy will help detect diabetes earlier and potentially lead to more effective treatment. However, the new guidelines will require physicians to perform the tests on individuals with at least one risk factor for diabetes.
The new guidelines recommend screening for both type 1 and type 2 diabetes in adults between 35 and 70 years old. The ADA also recommends lifestyle interventions to treat people with diabetes or prevent the disease. While screening for diabetes is one of the easiest ways to detect the disease, implementing prevention measures is more complicated. The USPSTF has found inadequate evidence that lifestyle interventions reduce the risk of type 2 diabetes. But, the recommendations are a step in the right direction and may make it easier to implement the new recommendations.
The ADA/EASD joint consensus statement includes recommendations for both type 1 and type 2 diabetes screenings. It also recognizes the need for genetic testing to identify individuals with diabetes. Screening for type 1 diabetes has been around for a while, and the concept of individualization in diabetes care is evolving to take into account the latest research. The new guidelines also include charts that help manage type 2 diabetes. It is possible to prevent the onset of serious health complications by early detection.
The standards for diabetes screening should include the prevention of microvascular complications and adherence to medication. This is especially important because diabetes increases the risk of Coronavirus SARS2 infection, which is known to increase the risk of new diabetes. Social determinants of health, such as income, education, and social support, are more influential in the outcome of diabetes than medical interventions. By incorporating agencies outside of the treatment team, diabetes screening can help prevent costs related to medication non-adherence.
Treatment

The American Diabetes Association (ADA) recently released its new diabetes treatment guidelines, the 2021 Standards of Medical Care for People With Type 2 Diabetes. This document includes new recommendations and updates from the ADA's Professional Practice Committee. The guidelines include information on prevention of type 2 diabetes, therapeutic approaches, and vaccine-specific updates. Learn more about the guidelines and how they will change the way you manage your patients. To learn more about the guidelines, watch this two-part podcast.
In developing the new guidelines, the USPSTF commissioned a systematic review of the available evidence on interventions for prediabetes and type 2 diabetes. The review focused on the benefits and harms of screening and other interventions, including pharmacologic treatment, behavioral counseling, and blood pressure and lipid control. The guidelines suggest that screening for diabetes and other chronic diseases should begin when a patient is 35 years old. However, the duration of follow-up was not long enough to detect a significant effect on health outcomes.
The ADA recommends that people with a high BMI undergo a blood glucose test every three years. After that, testing for diabetes should be done every year. People with a high BMI should have regular blood glucose tests as part of their regular health maintenance. In addition, people with obesity or risk factors should have their HbA1c level checked at least once a year. This screening can help detect diabetes early.
Smoking and drinking alcohol are also important considerations. Smoking can increase the risk of developing diabetes, so it is important to quit. Alcohol can also raise or lower blood sugar. It is best to drink a small amount of alcohol with meals to avoid dangerous effects on blood sugar levels. Also, people with diabetes should avoid chromium supplements, as they have only a few benefits. Excessive amounts can lead to kidney damage, muscle problems, and skin rashes.
The guidelines also recommend that adults with type 2 diabetes engage in 150 minutes of aerobic exercise a week. Resistance exercise should be done at least two to three times a week. Children should engage in activities that build strength and balance. In addition to aerobic exercise, the guidelines recommend that people with type 2 diabetes also engage in resistance exercise. The guidelines suggest that children should participate in exercises that involve the use of free weights, such as calisthenics.
Cost

Despite recent increases in healthcare costs, prescription drugs are still an important part of the cost of diabetes care. Many patients are forced to pay co-pays that can reach $200 a month. Fortunately, many drug manufacturers have patient assistance programs to provide free medications to qualified patients. Another option is the Partnership for Prescription Assistance, a free program offered by many pharmaceutical companies. Families can visit the American Academy of Family Physicians for recommendations. Doctors who are board certified in internal medicine can serve as primary care providers.
According to the latest report by the American Diabetes Association, the cost of diabetes care per capita has increased tenfold since 2007. The greatest increases are associated with insulin and medical equipment. However, this shift suggests progress in controlling chronic complications and potential targets for intervention to decrease ambulatory costs. However, the current guidelines do not include an estimate of what these guidelines will cost in 2021. Until then, the cost of diabetes care remains an unaffordable burden for many families.
The burden of diabetes is also substantial on society. This estimate excludes intangible costs such as pain, resources used by non-paid caregivers, and the costs associated with undiagnosed diabetes. But it is important to note that diabetes is not an isolated problem, as a significant number of people suffer from it. Those who have it are prone to complications and must undergo a variety of tests. Nevertheless, they are still under-diagnosed and incur higher costs.
The cost of diabetes care is one of the largest challenges faced by health systems, insurers, and communities. Currently, the cost of diabetes care has not been managed, but scientific studies are beginning to reveal what works best to contain costs and prevent harm. The new guidelines will also help in determining which diabetes treatments are best suited for individuals with diabetes. So, it is imperative that the American Diabetes Association continues to focus on this important issue.
A major concern is the cost of maintaining low-risk patients, particularly in the elderly. This is a fraction of the cost of treating acute complication, such as myocardial infarction. And the cost of keeping moderate-risk patients is not far behind. That cost difference may be worth millions of dollars over the next several decades. A cost analysis is important to guide policymakers. If the cost of diabetes care is increased, the benefits could outweigh the costs.










