If you are looking for treatment options for diabetes insipidus, you should know that there are many options available for this condition. Listed below are the symptoms, treatments, and imaging tests that may be performed. You should also be aware of the possible complications associated with diabetes insipidus. If you have any of these symptoms, or suspect you may have the condition, you should consult with your doctor. Alternatively, you can take the medicine desmopressin, which helps your body produce and use ADH. Desmopressin comes in a pill, a nasal spray, and a shot. It is important to take the medication as directed. You may experience dizziness or vomiting after taking desmopressin.
Causes
Diabetics with diabetes insipidus produce 20 quarts of urine per day. This is twice as much as the average healthy person produces. If your urine production becomes excessive, consult your doctor for further testing. Although diabetes insipidus may not be as dangerous as other types of diabetes, it should not be ignored. The symptoms of diabetes insipidus may be mild and unnoticeable unless they cause you to stop drinking water. Symptoms and signs vary from person to person, but if your symptoms persist, see your doctor for a proper diagnosis.
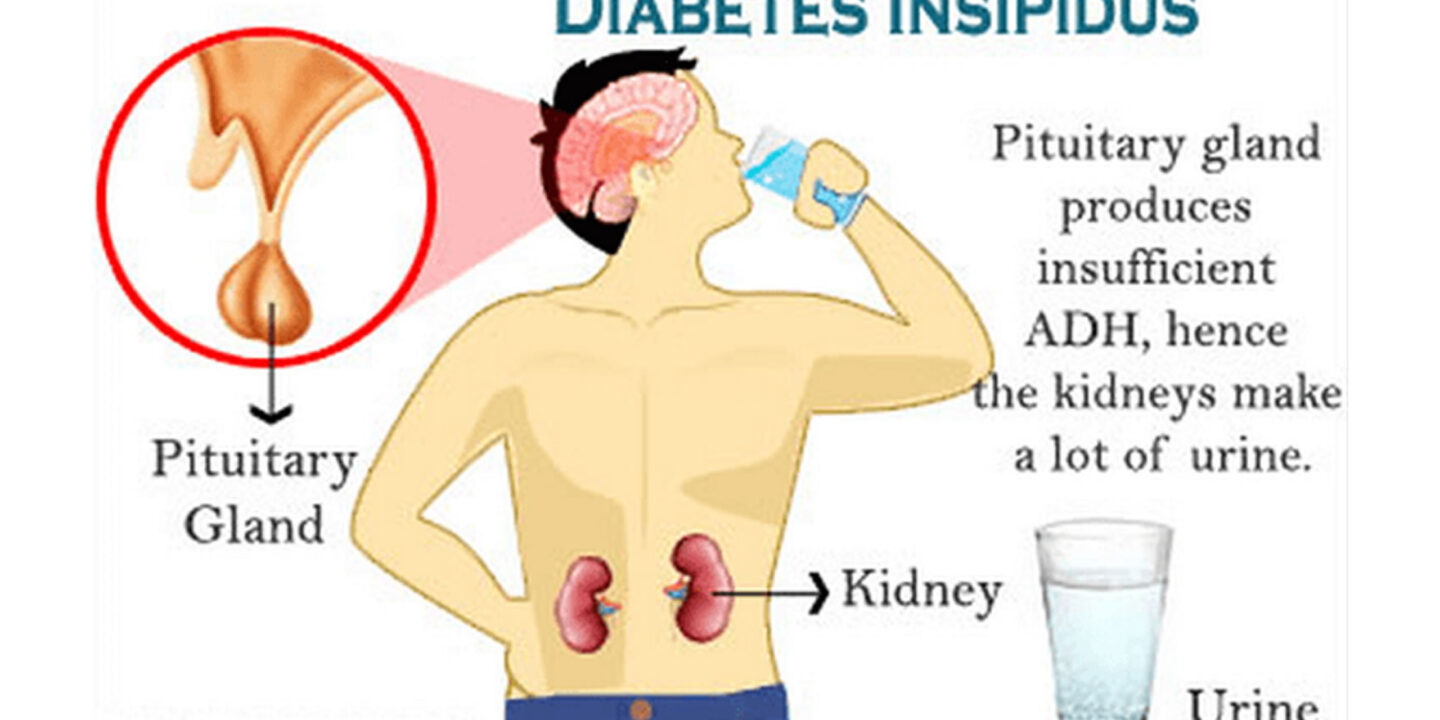
The main cause of diabetes insipidus is the malfunctioning of the antidiuretic hormone (ADH), which is produced in the hypothalamus and stored in the pituitary gland. Vasopressin regulates the levels of water in the blood and controls the volume of urine. Hence, when you have diabetes insipidus, you lose a massive amount of water through your urine, which can lead to dehydration or electrolyte imbalance.
Other potential causes of diabetes insipidus include head trauma, pituitary disease, or genetic defects. Although rare, inherited diseases such as a hypothalamic or pituitary tumor are the most common cause of diabetes insipidus, many people have it without even knowing it. Occasionally, CDI is caused by a mutation in one of the genes for the production of anti-diuretic hormone. The pituitary gland and hypothalamus are extremely susceptible to damage.
Other causes of diabetes insipidus can include certain medications. For example, lithium and tetracycline can cause diabetes insipidus. Your GP can prescribe an alternative medication, such as desmopressin. But if your condition is due to a physical condition, it is better to consult an endocrinologist than to stop taking the medication without a physician's advice.
The main symptoms of diabetes insipidus are extreme thirst and excessive urination. These symptoms occur because the pituitary gland produces too little of an antidiuretic hormone (ADH), or the kidneys fail to respond appropriately to the hormone. Patients with diabetes insipidus need to drink plenty of water, and they should also take medications to stay hydrated. In addition to water, people with diabetes can also drink plenty of coffee or tea.
Treatments
Diabetic insipidus is caused by problems with the hypothalamus and pituitary glands. Hypothalamus issues may be caused by a genetic mutation or head trauma, and pituitary gland problems can be a result of infection or tumors. A urine sample can be collected at home and sent to a lab for analysis. If the patient's urine has high concentrations of sodium, diabetes insipidus may be a complication of this problem.
One treatment for diabetes insipidus is fluid restriction. This method, based on trial and error, is designed to limit the amount of fluids a patient loses through urination. The fluids should be reintroduced at a rate of one gram per 100 milligrams of vasopressin. However, the treatment is not permanent. If the symptoms are mild and do not require frequent visits to a doctor, dietary changes may be sufficient.
A synthetic version of the hormone ADH is also available as a pill, nasal spray, or injection. The main goal of desmopressin treatment is to suppress the production of urine and relieve thirst. But this medication does have side effects, such as making the patient weak and dizzy. For these reasons, the patient should not drink too much water, as it can make him dizzy and weak. The treatment for diabetes insipidus should be individualized.
Medications for diabetes insipidus include lowering sodium levels in the diet and increasing water intake. Certain medicines, such as lithium, can also cause diabetes insipidus. Patients should not use too much salt, because this can cause dehydration. For mild cases of diabetes insipidus, increasing water intake may suffice. Thiazide diuretics, on the other hand, can reduce the production of urine by reducing ADH levels. Patients should consult a physician if these medications are not effective.
Diabetic insipidus is a disorder characterized by polydipsia and polyuria. The main cause is reduced secretion of vasopressin, a hormone responsible for controlling body fluid levels. Other causes include kidney failure, certain drugs, or chronic conditions. Diabetes insipidus is often diagnosed after ruling out other conditions. Symptoms and treatments for diabetes insipidus vary.
Imaging tests
Imaging tests for diabetes insipidus may help the doctor to determine whether the condition is caused by damage to the pituitary gland or hypothalamus. Another type of test is a water deprivation test, which involves not drinking liquids for several hours. The results of this test may indicate whether you have diabetes insipidus or primary polydipsia, a condition that causes excessive fluid intake. Imaging tests can help the doctor determine the exact cause of the condition and determine what type of treatment is needed.
Diabetic insipidus is a rare disorder of water homeostasis that results in an excessive loss of water in urine. AVP deficiency requires the destruction of over 90% of vasopressinergic neurons in the hypothalamus and posterior pituitary to result in diabetes insipidus. AVP deficiency is a hallmark of central diabetes insipidus, while nephrogenic diabetes insipidus occurs because of impaired renal concentrating capacity.
In central diabetes insipidus, the patient's urine is very dilute. Vasopressin injections stop urine production, indicating a deficiency in vasopressin. However, this procedure does not correct nephrogenic diabetes insipidus, where urine remains dilute and blood pressure does not change after vasopressin injection. MRI scans may also reveal lesions in the pituitary gland.
Patients with diabetes insipidus should be closely monitored during the fasting period, as dehydration may result without adequate dDAVP. Patients should also be given maintenance isotonic fluids throughout the fasting period. Frequent blood sodium checks should be performed at regular intervals. However, patients should avoid overzealous intravenous fluid administration. This can lead to hyponatremia.
In some cases, the symptoms of diabetes insipidus are accompanied by peripheral symptoms, such as thirst and phlegm. MRI tests can detect the presence of peripheral or central diabetes insipidus, or a combination of the two. The most common imaging test for diabetes insipidus is a multi parasitic magnetic resonance imaging (MRI).