
Women with GDMA1 are more likely to have osteoprotegerin than non-cases. CT allele carriers also have higher OPG. The high BMI of GDMA1 women was found to be a significant contributor to increased OPG. The distribution of the CT genotype was also higher among women who were multiparous.
Placental pathology in gdma1
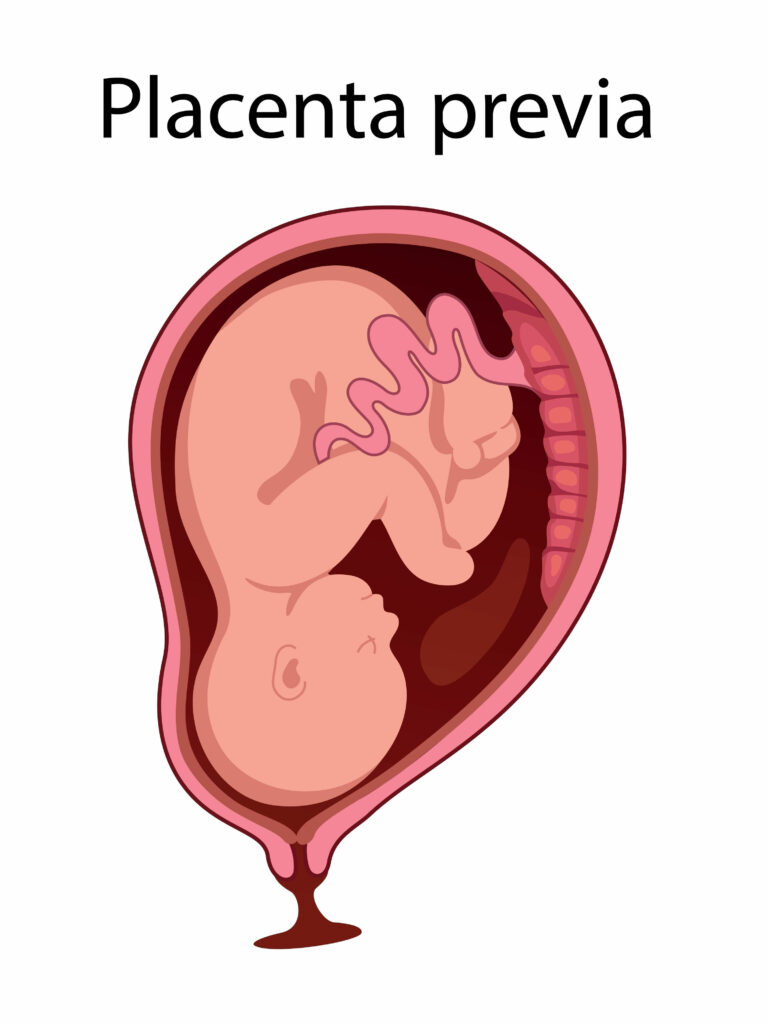
The placenta is a poorly studied organ. Understanding its immunobiology can help answer important questions regarding transplant biology and autoimmune diseases. The pathology of the placenta involves insults to the maternal and fetal vascular compartments and the placental itself. The presence of these insults affects the placenta's reserve and can lead to serious consequences for the fetus.
Placental tissues were obtained from a microtomy of the placental bed and prepared for histopathological analysis. The samples were fixed in formalin and dehydrated in a graded ethanol series. The placentas were then sectioned at 5 mm and evaluated under a light microscope. The tissue was then stained with hematoxylin and eosin.
Placental pathology in GDMA1 and GDMA2 women was similar. The OAV group had a higher rate of FVM lesions, which indicates impaired placental function. However, the groups had similar rates of CD and adverse neonatal outcomes.
Placental pathology in gd ma1 is characterized by a large percentage of in-utero infections. The placenta acts as a barrier against most infections, but some infections can reach the placenta and fetus. In some cases, these infections may result in congenital infections, which affect both the mother and the child.
Placental pathology in gd ma 1 patients varies according to gestational age and severity of maternal diabetes. Placental abnormalities include an increased incidence of villous immaturity, increased measures of angiogenesis, and an increased weight of the placenta. The different placental lesions may reflect differences in the pathophysiology of diabetes in the two groups.
Placental pathology in gd ma1 patients shows multiple histological changes, with the most common changes affecting the placenta. MGH placentas have higher rates of syncytial nodes and endarteritis than GDM women. In addition, women with GDM placentas had fewer calcification and a decreased incidence of syncytial nodes.
Prenatal care for women with gdma1

Women with GDMA1 are at increased risk for gestational diabetes mellitus. Although the exact relationship between this condition and fertility treatments is unclear, some studies have demonstrated an increased risk for GD among those who successfully conceive through fertility treatments. In a population-based cohort study, women with GDMA1 who conceived spontaneously or after fertility treatments were evaluated for perinatal outcomes and pregnancy complications.
Outcome-based criteria for the diagnosis of gdma1

The study's authors report a low incidence of pregnancy complications in women with GDMA1 and lower rates of cesarean delivery. These findings may be due in part to a study that analyzed women's records of perinatal and neonatal outcomes. The study also found that women with GDMA1 are less likely to have preeclampsia and intrauterine growth restriction, which are associated with increased risk for adverse pregnancy outcomes.
In the study, the IADPSG convened a consensus panel to develop diagnostic criteria for GDM. The panel considered multiple strategies for diagnosis and recommended a standardized diagnostic process. Its findings should help health-care providers choose the best screening approach for GDM.










