
The IFCC hba1c is a biomarker for diabetes that reflects the real HbA1c concentration in patient samples. It is not a realistic model for clinical laboratories, and it increases with age. For these reasons, this biomarker is rarely used to diagnose diabetes.
Table of Contents
IFCC hba1c is a biomarker for diabetes
HbA1c is an important biomarker of diabetes, which can help physicians determine whether a patient has diabetes or not. This measurement correlates with the levels of blood glucose, plasma insulin, C-peptide, and autoantibodies, which are all essential for diagnosis and subtype classification of diabetes. There is a need for more standardization of diabetes biomarkers to ensure that they are comparable and accurate across laboratories.
Although HbA1c is a highly useful biomarker for diabetes, it is less accurate in some people, especially patients with diabetes who also have anemia. It also tends to underestimate the degree of glycemic control in patients with anemia. Moreover, the level of HbA1c increases in diabetic women during pregnancy, particularly during the third trimester.
HbA1c is measured as a ratio of total hemoglobin to HbA1c. To calibrate the IFCC hba1c, a calibration mixture of highly purified HbA1c was used. It was assessed and approved by an international network of reference laboratories in July 2001. This method is based on the concept of metrological traceability. It is used to assign HbA1c values to whole blood panels that serve as a calibration for manufacturers.
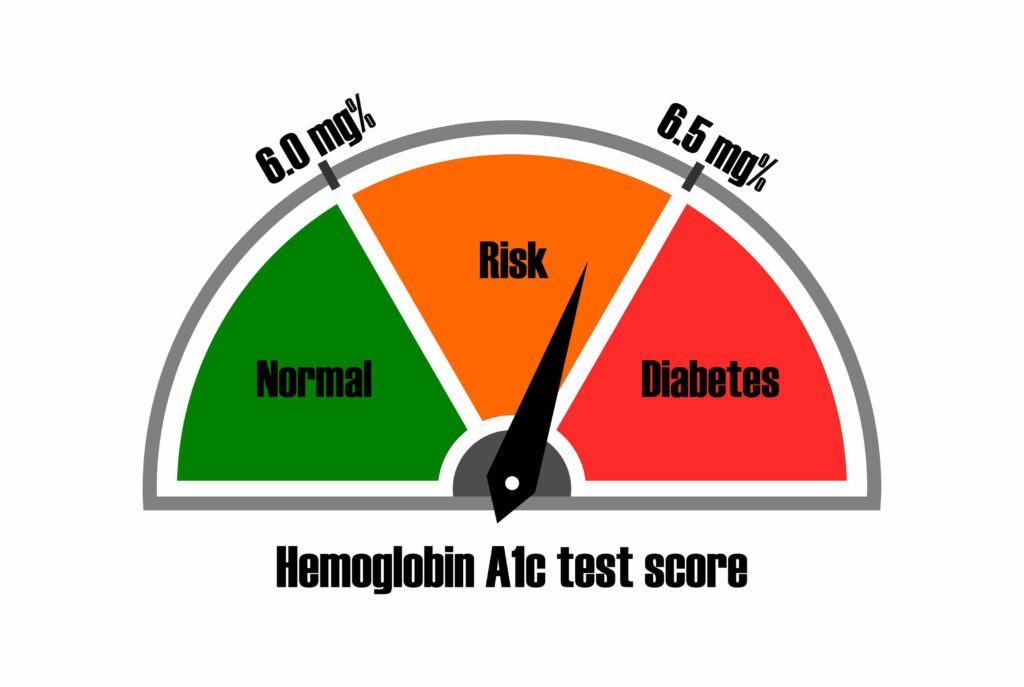
HbA1c is a useful biomarker of diabetes and can help physicians monitor chronic hyperglycemia. High levels of the biomarker are linked to the development of cardiovascular disease. The American Diabetes Association recommends an HbA1c value of >6,5 percent be used as the cutoff for diagnosing diabetes. Those with values between 5.7 and 6.4% are considered prediabetic.
It reflects true HbA1c concentrations in patient samples

The IFCC HbA1c is a non-enzymatic method used to measure the average HbA1c concentration in patient samples. It is considered more accurate than other methods of measuring HbA1c because it is less expensive, quick, and sensitive. It is often used in diabetic patients for glycemic control monitoring.
The IFCC HbA1c unit is more scientifically valid than the NGSP unit, because the IFCC system reflects true HbA1c concentration in patient samples. The IFCC unit is also more precise than the NGSP unit. This is important because HbA1c concentrations in patient blood samples range from five to 10 mmol/L.
The IFCC HbA1c test results are interpreted using the sigma-metrics approach, which considers biological variation. The criterion for TAE is set at 5 mmol/mol (0.46%). If a patient's HbA1c concentration falls below the TAE criterion, then the patient should be re-evaluated.
There are many potential reasons why a patient's HbA1c levels might be higher than the true value. This can include chronic kidney disease or severe hyperbilirubinemia. There may also be interferences in the laboratory assays.
A major drawback of the IFCC HbA1c method is the time lag. The median time-lag was two to four days, and the difference was not related to the difference between the central and local measurements.
It is not realistic for clinical laboratories

Ifcc HbA1c is a test that measures the average blood sugar levels in people with diabetes. The results of the test are typically reported on one scale. This makes it difficult to compare the results with other laboratory tests. But it does offer a few advantages. First, it has lower CVs than most other clinical tests. In fact, the CV for cHbA1c is lower than that for FPG or 2-h PG.
Second, cHbA1c is superior to laboratory HbA1c. It is more accurate and can be used in clinical practice. Moreover, it minimizes patient inconvenience. The occurrence of blood tests can cause anxiety, especially in younger patients. Moreover, cHbA1c can be performed electronically, avoiding direct patient contact. In a COVID crisis, social distaging can be reduced by using this technology.
In addition to cHbA1c being more accurate than laboratory HbA1c, CGM-derived HbA1c has a smaller deviation than laboratory HbA1c. This means that there are less clinically relevant deviations with cHbA1c, which may alleviate the patient's concern.
It is important to have high accuracy in HbA1c measurements. It is critical for diabetes diagnosis and monitoring. As a result, it is important for clinical laboratories to closely monitor the performance of their methods.
It increases in obese and lean individuals

In two population-based studies, HbA1c concentrations were positively related to age and obesity. Overweight and obese individuals had higher HbA1c concentrations than lean and normal-weight individuals. The association persisted even after accounting for body fat percentage and age.
Obesity is associated with an inflammatory state and an altered metabolic profile. These changes were a result of higher glycated hemoglobin levels and increased levels of high-sensitive C-reactive protein. This change was more pronounced in obese individuals than in lean individuals.
Compared to patients with a low-BMI, severe obesity was associated with increased risk of heart failure. However, individuals with optimal glycemic control had a lower risk of heart failure. Despite these associations, BMI and AMI did not appear to be independent predictors of heart failure.
Although HbA1c is a reliable biomarker for glucose control, it also has some limitations. There are many confounding factors that affect the results. For instance, smoking and obesity are risk factors that may increase the risk of developing diabetes.
It is unaffected by short-term hormonal surges
Short-term hormonal surges do not affect the measurement of HbA1c levels. This blood marker has a high degree of stability and low variability at 37degC. This makes it easy to test symptomatic patients on their first visit. However, some health conditions, such as anemia, can falsely increase or lower the levels. It is generally measured in percent or mmol/mol.
The HbA1c level may vary by season, ethnicity, and pregnancy. It may also depend on a woman's genetic makeup and concurrent diagnoses. Nonetheless, in a healthy pregnancy, HbA1c levels should remain close to normal.
The findings of this study suggest that the HbA1c test may continue to be a helpful diagnostic and prognostic tool in clinical practice. This finding may lead to improved patient care and successful clinical outcomes. For now, it remains unclear how these findings will affect the future of this test.
In two independent population-based cohorts, HbA1c levels were positively associated with age. They also increased in overweight and obese individuals. However, this association remained unchanged after the exclusion of obesity and medication. These results can be transferred to other centres and may improve patient care.










