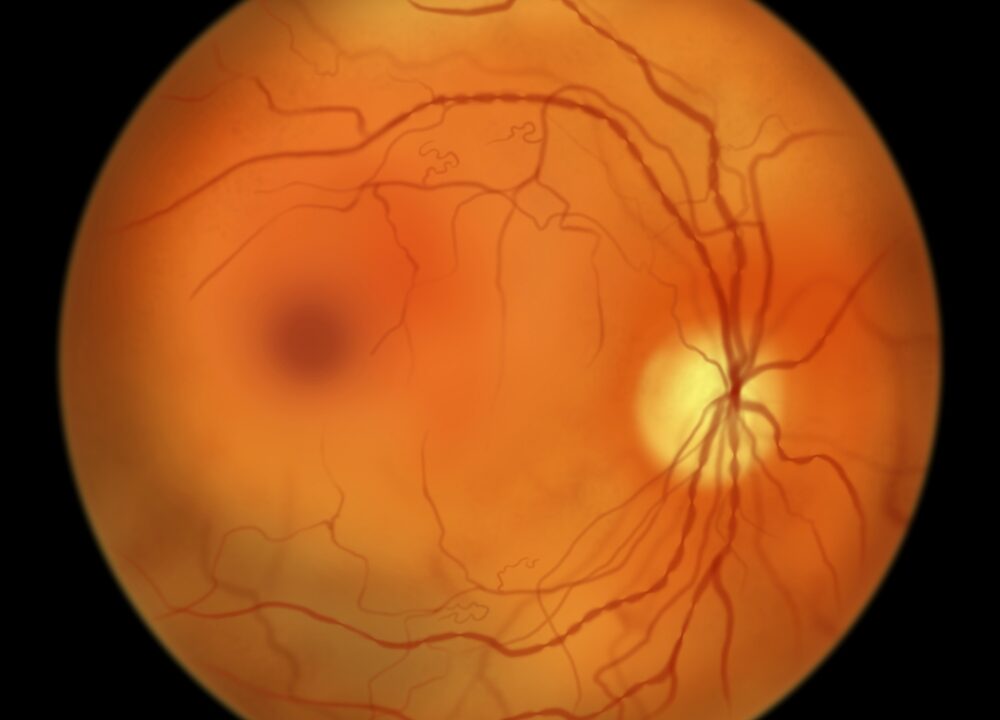
Non proliferative diabetic retinopathies are characterized by changes in the blood-retinal barrier. These changes are associated with an increased risk of progression. In one study, Silva et al. found a fourfold increase in the risk of progression in patients with peripheral lesions. Other changes include neovascularization and macular edema.
Table of Contents
Changes to the blood-retinal barrier
Non-proliferative diabetic retinopathy is associated with changes to the blood-retinal barrier and changes to retinal thickness. This process can lead to significant visual impairment. This condition can also cause macula oedema. Ultimately, retinal neovascularization may lead to sight-threatening vitreous haemorrhage and tractional retinal detachment. The abnormal growth of new blood vessels in the retina is mediated by cytokines and vascular endothelial growth factor.
One study found that a high proportion of patients with non-proliferative diabetic retinopathy exhibited changes to the blood-retinal barrier. The most common alterations included RLA-leaking sites, areas of increased retinal thickness, microaneurysms, and drusen. In addition, hemorrhages were relatively rare.
Changes to the blood-retinal vascular system have been studied to improve noninvasive diagnosis of Alzheimer's disease (AD). Several vascular changes appear to be relevant to early brain pathogenesis and cognitive decline, suggesting a link with vascular amyloidosis and pericyte loss.
One pathway implicated in the pathology of non-proliferative diabetic retinopathy is the PI3K/Akt/mTOR pathway. Studies have shown that inhibition of mTOR inhibits the breakdown of the blood-retinal barrier. The mechanism of action of mTOR inhibitors is unclear, but it may be mediated by inhibition of downstream factors, including NF-kB, MCP-1, and TNF-a. Currently, several mTOR inhibitors are undergoing clinical trials.
A bio-reductive drug, pimonidazole, is introduced into animals. This drug forms insoluble adducts with tissue proteins and can be detected by an antibody. This antibody has the ability to localize these adducts. An antibody specific to pimonidazole-adducts is present in diabetic retinas.
In this study, researchers analyzed the changes in the blood-retinal barrier in non-proliferative diabetic retinopathy using an ETDRS protocol. These measurements were obtained by evaluating the density of capillaries adjacent to the avascular foveola and with a trypsin-digested preparation.
Researchers studied twelve nonproliferative diabetic retinopathy patients who were aged 44 to 63 years. The study population included patients with non-proliferative retinopathy, a mild form of the disease. The patients in the study had corrected vision acuity of 20/20.
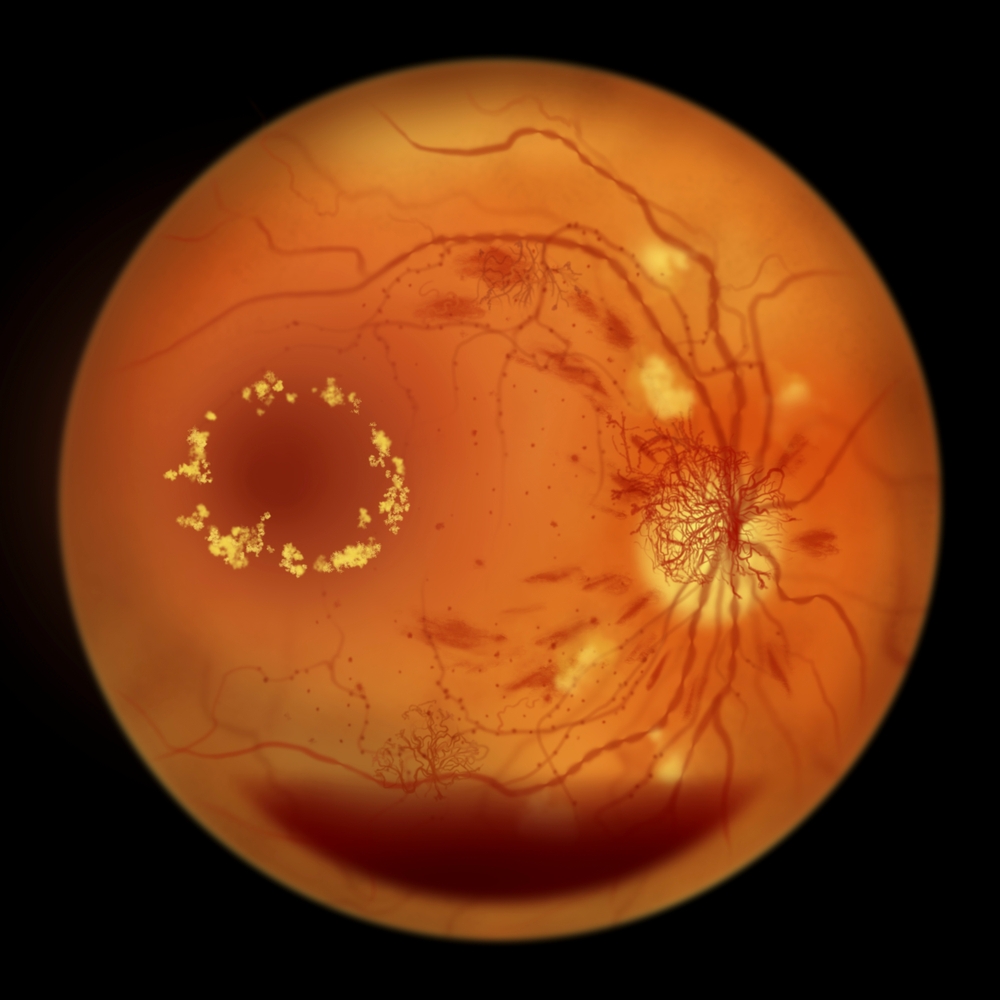
Neovascularization
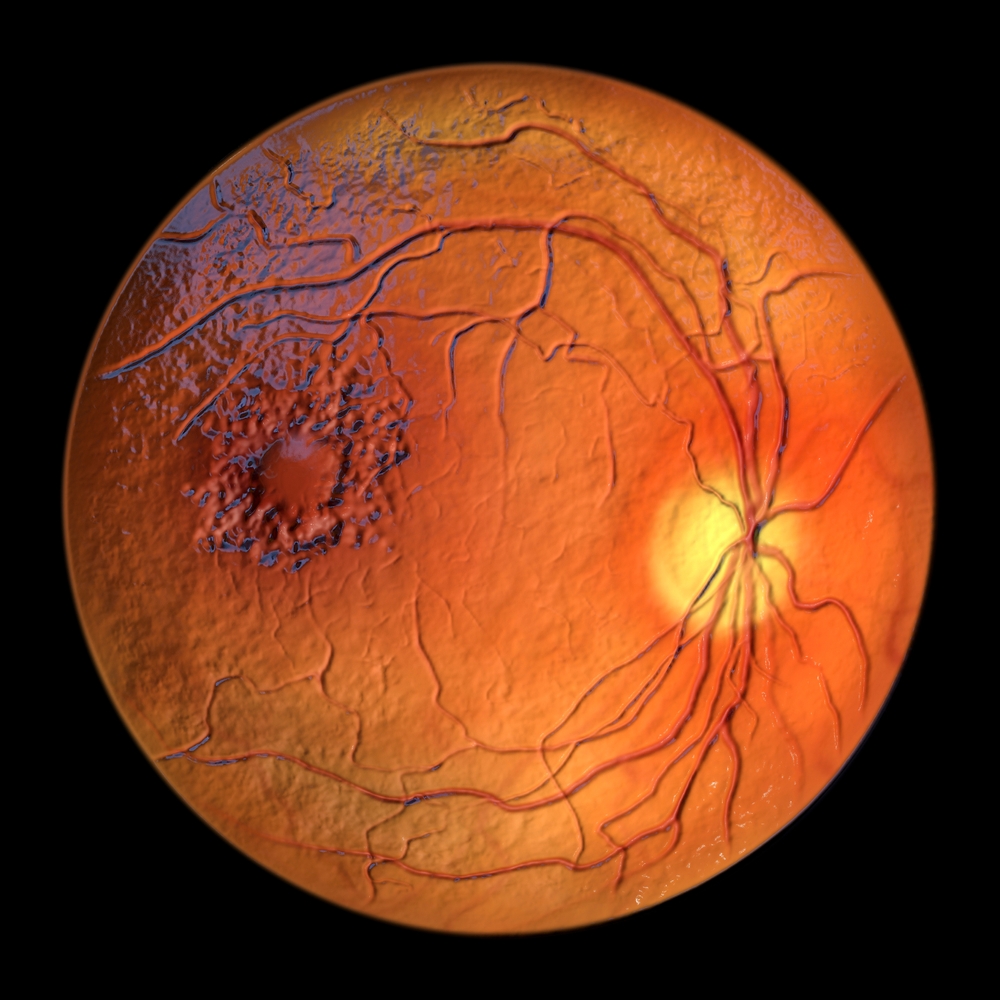
The symptoms of diabetic retinopathy include decreased vision loss. This condition is caused by microaneurysms that form in the central retina and leak fluid. The macula is the region of the retina that controls central vision, and even a slight damage to this region can lead to significant vision loss. Additionally, this condition can lead to scar tissue development and Vitreous Hemorrhage. Rarely, it can lead to Tractional Retinal Detachment, which is severe and can cause blindness.
The presence of neovascularization (NV) on repeat fluorescein angiography is a characteristic feature of proliferative diabetic retinopathic retinopathy. However, it is rare to detect neovascularization in routine histological sections. It is important to recognize NV early to prevent the disease from progressing to a more serious stage.
Diabetic retinopathy is the leading cause of blindness worldwide. It can be characterized by two types: proliferative diabetic retinopathic (PDR) and non proliferative (NPDR). Optical coherence tomography (OCT) is a noninvasive imaging method that has been shown to be helpful in assessing neovascularization in PDR. It can also detect intraretinal microvascular abnormalities, subhyaloid hemorrhages, and retinal nonperfusion regions.
Researchers from the Early Treatment Diabetic Retinopathy Study (ETDRS) reported on the long-term effects of laser photocoagulation for non-proliferative diabetic retinopathy. The results showed that the use of the treatment reduced the risk of developing diabetes-related vision loss in diabetic patients.
This disease can also result in moderate-grade neovascularization in the retina. In this stage, small blood vessels in the retina become blocked, reducing the amount of oxygen and nutrients that reach the retina. The condition has similar symptoms to non-proliferative retinopathy.
Neovascularization in non-proliferative diabetic retinopathy is characterized by the formation of new blood vessels that are ill-defined and characterized by poor structural integrity. The basement membrane is fragile, the endothelial cells are lacking in tight junctions, and the walls of these new vessels are porous. As a result, plasma proteins and hemorrhages can leak from these vessels and damage the retina.
Diabetes causes damage to blood vessels in the body, especially in small blood vessels. This leads to microaneurysms, focal areas of weak wall cells, and leakage. These vessels eventually close and clot, restricting oxygen and nutrients to the retina.
Macular edema
Diabetic retinopathy is a serious eye disorder that leads to the loss of vision. It is the third leading cause of vision impairment among adults over 40. While the condition is often asymptomatic, it can eventually progress to the extent of blindness and significant functional impairment.
It is critical to control blood sugar to prevent macular edema. Keeping a good blood sugar level is also important to keep other risk factors under control. If left untreated, diabetic retinopathy can lead to severe vision loss and blindness. It may require multiple focal laser treatments to reduce vision loss.
Diabetic retinopathy can cause macular edema, a swell of the macula. This edema is caused by fluid leaching from damaged retinal capillaries. In the worst cases, the condition may affect the central vision, though peripheral vision may remain intact. Treatment for macular edema may involve anti-VEGF medications and laser treatment.
Macular edema can be accompanied by other signs of retinopathy. A doctor can also conduct an optical coherence tomography scan to assess macular edema. This scan is useful for determining the cause of macular edema and develop a treatment plan.
There are several possible causes of macular edema. Nonproliferative diabetic retinopathy has several causes. The retina may be damaged from a number of factors that contribute to ischemia, including a faulty metabolic balance between endothelial cells and leukocytes. Some of these factors may also result in retinal microaneurysms.
Nonproliferative diabetic retinopathy (NPDR) is often accompanied by hemorrhages and microaneurysms. The macula no longer receives adequate blood supply. Although there is no cure for this disease, it can be treated using laser therapy.
Macular edema in non-proliferative diabetic retinopathy is characterized by abnormal thickening of the retina. Although it is not a life-threatening disease, it can result in significant vision loss in some people.
Anti-VEGF therapy is an alternative treatment for nonproliferative diabetic retinopathy. This procedure involves injection of a medication that binds to excess VEGF and eliminates it from the eye. Lucentis, for example, is a drug approved by the FDA for treating macular edema. There are also other drugs available, including Avastin and Eylea. Another option for treating nonproliferative diabetic retinosis is intraocular steroid injection, which can help reduce the amount of fluid that leaks into the retina. These treatments may require multiple sessions and are often combined with laser therapy to achieve the best results.
Vision loss

When people have diabetes, they may develop a condition called non-proliferative diabetic retinopathy. This condition causes vision loss because the retina is unable to receive enough blood. Over time, the amount of sugar in the blood causes the retina's tiny blood vessels to become blocked. This results in blurred vision and spots floating in the retina. New blood vessels can also form on the surface of the retina, causing the retina to bleed and obstruct vision.
The early stages of nonproliferative diabetic retinopathy are characterized by small swellings in the retina's blood vessels. These areas may leak a small amount of fluid, which causes swelling of the macula, which is the area of the retina near the center. In some cases, these abnormal blood vessels may even grow into the vitreous cavity, causing bleeding.
Diabetic retinopathy may be treated with injections to reduce the amount of blood that leaks from the retina. This may help slow down the progression of the disease, allowing the patient to continue with their daily routine and prevent further vision loss. Laser surgery can also be used to reduce the number of new blood vessels in the retina.
Early detection of diabetic retinopathy is important, because if left untreated, it can progress to proliferative diabetic retinopathies. Diabetic retinopathy is often diagnosed during an eye exam. The symptoms usually affect both eyes. If you notice any of these symptoms, you should see a doctor immediately to have your vision checked.
Diabetic retinopathy is a condition caused by too much blood sugar. The high blood sugar damages the tiny blood vessels in the retina and can lead to blurred vision. In severe cases, diabetic retinopathy may lead to irreversible loss of vision. Diabetic retinopathy can be prevented by having regular eye exams.
Diabetic retinopathy can be treated using laser surgery or medications to prevent the formation of new blood vessels. The treatment will depend on the stage of the disease and the severity of vision loss. Laser surgery can be used to seal leaking blood vessels, while medications can be used to decrease inflammation and prevent new ones. In advanced cases, the retina may have to be repaired surgically.










