
Alzheimer's disease and diabetes are connected through insulin resistance in the brain. Researchers are exploring the potential triggers of Alzheimer's disease in people with diabetes and Alzheimer's. Type 3 diabetes may be the key to early detection of this degenerative disease. A proposed term, “type 3 diabetes,” has been used to describe this connection between diabetes and neurodegenerative disease. Here are some facts about this disease. The best way to deal with it is to be aware of your risk factors.
Alzheimer's disease is caused by insulin resistance inside the brain

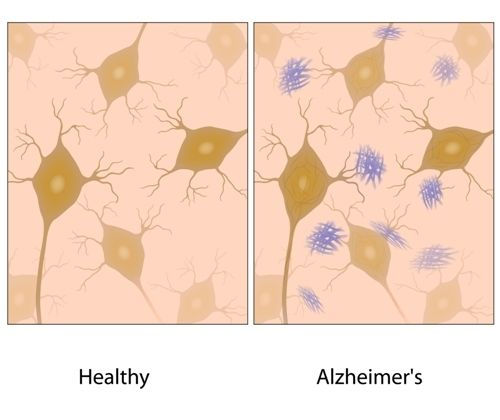
The proposed term for Alzheimer's disease is type 3 diabetes. Type 3 diabetes is not the same as type 3c diabetes mellitus, which can be a result of other pancreatic disorders. However, people with type 3 diabetes have a 65% greater risk of developing Alzheimer's. Type 3 diabetes affects the brain in a variety of ways, including damage to neurons, impaired glucose metabolism, and amyloid plaques.
One of the common causes of dementia is insulin resistance. About 81 percent of individuals with type 2 diabetes also have the disease. Insulin resistance causes cells to not respond to insulin. This is bad for the brain because the brain uses enormous amounts of glucose. Insulin resistance also affects peripheral tissues. It impairs working memory networks, leading to cognitive decline. For this reason, researchers have been studying the relationship between diabetes and Alzheimer's disease.
The study also identifies a genetic risk factor that is linked to Alzheimer's. People with this risk factor carry a type of APOE called E4, which is associated with approximately 50 percent of Alzheimer's cases. A new study published in the journal Neuron outlines the study's findings. For journalists and medical professionals, there's a broadcast-quality video pkg of the study. A script is also included in the package.
Treatment is insulin-sensitizing agents

Insulin-sensitizing agents are one of the treatment options for Type 3 diabetes. These drugs can improve blood sugar control by reducing the amount of insulin secreted into the bloodstream. Metformin and other diabetes drugs that pass the blood-brain barrier have been tested for their potential AD activity. Although the results are not yet clear, some researchers suggest that insulin-sensitizing agents may have beneficial effects on AD symptoms.
The non-insulin agents are also available. These drugs do not cause significant hypoglycemia and are therefore safe for peripheral administration. Insulin-sensitizing agents are also used in people with type 2 diabetes. However, these drugs do have side effects. Because they do not produce insulin-like effects, they are not recommended for everyone with type 3 diabetes. For those who wish to avoid the risks associated with these drugs, metformin may be a better option.
Alzheimer's disease is a chronic neurodegenerative disease

The incidence of Alzheimer's disease is increasing around the world, with the number of people with diabetes reaching the highest level in several countries. This neurodegenerative disease is characterized by memory loss, impaired cognitive function, and difficulty with daily activities. There is no known cure for this disease, but the disease's pathology has been well studied. Its mechanisms include beta-amyloid plaque formation and the neurofibrillary tangles made up of tau protein. As a result, this disease is a leading cause of dementia among the elderly. However, no effective cure has been discovered for this neurodegenerative disease.
The term Type-3-Diabetes refers to the condition, which shares some pathological and molecular characteristics with Type-1 and Type-2 diabetes. One of the key factors for Type-3-Diabetes is insulin resistance. Insulin is essential for proper glucose regulation, and poorly controlled blood sugar contributes to the development of Alzheimer's. Insulin resistance causes bioenergetic dysregulation, which promotes the progression of Alzheimer's disease.
Diabetics with poor glucose control are at a greater risk for dementia. The earlier diabetes starts, the greater the risk of developing dementia. Uncontrolled blood sugar can lead to the accumulation of neurotoxins and increased stress on neurons. Ultimately, diabetes and dementia are closely related. While there is no proven cure for Alzheimer's disease, type 3 diabetes can provide proactive therapeutic strategies for patients. In the future, anti-T3D drugs with cognitive effects may help prevent dementia in patients.
Gestational diabetes is a risk factor for Alzheimer's disease

While gestational diabetes is often asymptomatic, the high glucose levels that are a common part of pregnancy can affect the baby and the mother. If not managed properly, gestational diabetes can cause the baby to grow to be large, leading to a higher risk of complications such as birth injuries and a C-section. Pregnant women with diabetes are also at greater risk of preterm birth and early labor. If the baby is too big for the mother, early delivery is recommended.
Diabetes and Alzheimer's disease are closely connected. Studies have shown that diabetes has an increased risk of dementia, while elevated glucose levels can cause Alzheimer's disease. The disease is also associated with a higher risk of preeclampsia, an abnormality of pregnancy that causes high blood pressure and protein in the urine. In some studies, these factors have been linked to cognitive decline, which is associated with a lowered brain's ability to function correctly.
Type 1 and type 2 diabetes can increase the risk of Alzheimer's disease. Type 1 diabetes is caused by an inability to produce enough insulin in the pancreas. Type 2 diabetes results from the body becoming resistant to insulin. Type 3 diabetes is believed to increase the risk of Alzheimer's disease. This disease can cause a woman to have a higher risk of Alzheimer's disease.
Over consumption of foods that mess with insulin's many roles
Diabetes has two types: Type 1 is inherited and type 2 is acquired. Type 2 is commonly associated with the overeating of the United States. Since the early 1980s, diabetes has spread from adults to children. Research on the link between type 2 diabetes and Alzheimer's disease is getting more convincing. Diet is one of the leading causes of both diseases. This article will outline the link between diabetes and Alzheimer's disease, and discuss a few of the foods that may increase your risk.
Sugary commercial sweet foods are high in saturated fat. Saturated fat increases blood cholesterol levels and increases the risk of heart disease. The human body uses carbohydrates to produce energy, which is carried throughout the blood and delivered to all cells. To keep glucose levels constant, the body has developed systems that ensure this supply of energy. One of these systems is insulin, which is secreted by the pancreas.
Amyloid beta protein deposits in the pancreas are similar to amyloid beta deposits in the brain
The structure of both IAPP and Ab proteins is similar to that found in AD and diabetes. Because of this similarity, new therapeutic approaches targeting both proteins may lead to more effective compounds. Further evidence of synergy in these two diseases would alleviate the number of people who suffer from them, as well as the economic burden of these chronic maladies.
The amyloidogenic proteins that cause Alzheimer's disease and diabetes share a common structural motif. The similarities between the brain and the pancreas led to the development of several classic eponymic diseases. The similarities are striking, as the two are both characterized by amyloid deposits and abnormal beta-pleated sheet architecture.
In a recent study, scientists examined the brain and pancreas of 21 people with Alzheimer's disease. Amyloid beta protein was present in all the brains of the individuals studied, and it was co-localized with amylin. Beta sheets were detected using infrared microscopy. These findings indicate that amyloid beta deposits in the brain and pancreas may be related to each other.
Studies of human AD patients found that amylin deposits were present in the temporal cortex of the brains of diabetic patients as well as healthy controls. Interestingly, these deposits were found to be present in brain tissue from patients with diabetes and Alzheimer's disease. Amylin deposits were found in a high percentage of the diabetic subjects studied in the ACCORD-MIND study.










