What are some of the types of treatments for type 2 diabetes available on the NHS? These treatments include Insulin injections, Weight loss surgery, and SGLT-2 inhibitors. Despite the many options available, each one has its own risks and benefits. This article explores some of them in more detail. The NHS DPP is an example of a treatment that uses behavioural intervention to help people with NDH reduce their risk of developing Type 2 diabetes.
Table of Contents
SGLT-2 inhibitors
The effectiveness of SGLT-2 inhibitors for the treatment of type 2 diabetes has been well documented in the literature. These agents have shown efficacy as monotherapies as well as when used in combination with insulin or other oral antidiabetic drugs. In clinical studies, all three agents have shown similar efficacy. The available evidence suggests that SGLT-2 inhibitors are a promising alternative to sulfonylureas.
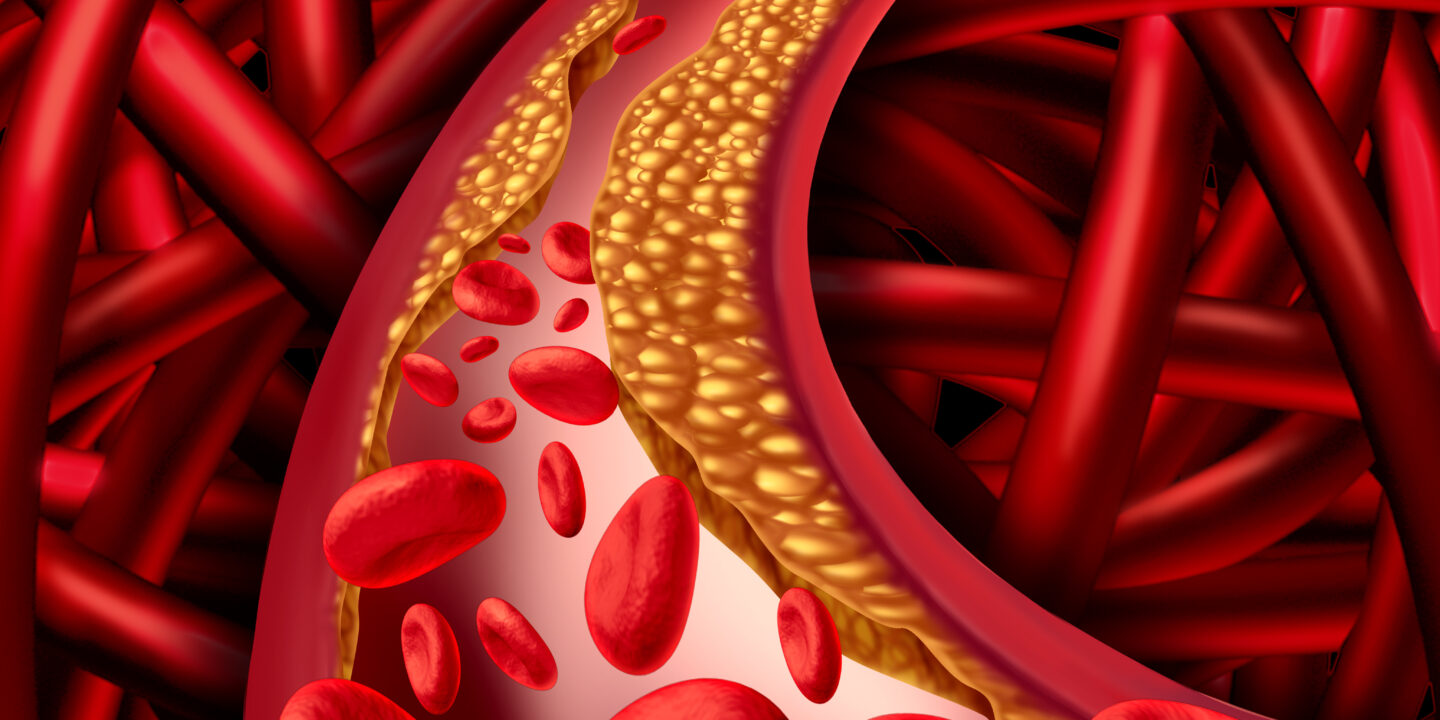
SGLT-2 inhibitors are associated with a variety of complications, including diabetic ketoacidosis, an infection characterized by elevated blood acidity. Diabetic ketoacidosis can be a life-threatening condition, and patients should be educated on its symptoms. Some SGLT2 inhibitors are associated with an increased risk of developing diabetic ketoacidosis (DKA), a condition in which blood sugar levels have reached dangerously low levels.
Although SGLT2 inhibitors are not effective for the treatment of type 1 diabetes, they may offer an advantage for patients with diabetes and other risk factors. Researchers have found that SGLT2 inhibitors can improve blood glucose control and blood pressure, as well as reduce the risk of cardiovascular disease and death. While they are not recommended for use in children or patients with Type 1 diabetes, they are appropriate for use in adults.
SGLT-2 inhibitors are associated with a decreased risk of heart failure. A 2018 review found that these drugs reduced hospitalization rates by 23 percent irrespective of cardiovascular history. In addition to improving the treatment of type 2 diabetes, SGLT2 inhibitors can also be beneficial for individuals without type 1 diabetes. The drug has been used for more than 15 years and has been approved for this purpose. It is currently the most effective type of insulin-independent diabetes treatment.
Weight-loss surgery
The goal of weight-loss surgery for type 2 diabetes is to reduce body weight and control blood sugar levels. In the past, surgery was reserved for people with severe obesity and no medical condition that would benefit from it. However, advances in surgery have led to new possibilities. Some types of metabolic surgeries, such as bariatric surgery, can benefit patients with diabetes who are nonobese. Here are some of the main benefits.
The surgical procedure has been effective in improving patients' health. Almost 90% of obese patients in a recent study achieved complete resolution of their type 2 diabetes. Their fasting blood glucose and hemoglobin A1c levels improved. In addition, their hyperlipidemia, osteoarthritis, and obstructive sleep apnea improved significantly. In another study, Schauer et al. (17) found similar results for 1,160 obese patients. Of these patients, 240 had type 2 diabetes or impaired fasting glucose.
One study in the New England Journal of Medicine reported that Roux-en-Y gastric bypass has been more effective than other gastric bypass procedures. Patients who undergo the surgery lose between 50 and 80% of excess weight within 18 to 24 months. Furthermore, the effects on blood sugar levels are immediate. Furthermore, 33% of patients don't need diabetes drugs after the surgery. Furthermore, 83% of these patients no longer need any diabetes medication after two years.
Insulin injections
For type 2 diabetes treatment, your doctor may prescribe insulin injections. You may need to take one or more insulin injections daily, or you may be prescribed both short-acting and long-acting insulin. The dosage of each type of insulin will be adjusted according to your blood sugar levels. Typically, insulin dosage is increased or decreased by two to three units every three to seven days. You should follow your doctor's schedule for insulin administration to avoid unwanted side effects.
The best location for an insulin injection is usually the abdomen, in a semi-circle under your belly button, or the sides of your thighs and bum. However, you must rotate the injection sites, since the body absorbs insulin at different rates. The abdominal region, for example, absorbs insulin faster than the leg or arm. The absorption rate may also vary depending on the amount of fat in the area. The more fat under the skin, the slower insulin is absorbed by the body.
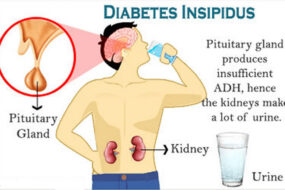
Before beginning insulin therapy, it's important to understand how the disease works. A1C levels measure your blood sugar levels on average over a two to three-month period. A1C levels of seven percent or less are considered good targets for treatment. Higher A1C levels may warrant an even more intensive medication regimen. Symptoms of type 2 diabetes include excessive thirst, frequent urination, and weight loss. Your doctor may prescribe insulin treatment to manage the symptoms of this condition.
SGLT-2 inhibitors in pill form
If you're considering taking SGLT-2 inhibitors in pill form to treat your type 2 diabetes, you may be wondering if they're right for you. The FDA doesn't approve these drugs for people with type 1 diabetes, and they may increase your risk of serious side effects like diabetic ketoacidosis. In addition, if you have severe kidney damage, you should avoid these medications. And while they're great at reducing blood sugar, they can also raise your risk of urinary tract infections.
SGLT-2 inhibitors in pill form aren't an alternative to insulin, but they can lower blood sugar levels by a small amount. But if you're uncomfortable with insulin shots or don't want to take insulin every day, this type of medication might be right for you. It can also help you lose weight, if you're looking for a way to lower your sugar levels without the need for insulin.
Besides lowering blood sugar, SGLT2 inhibitors also improve foot health. Currently, there are four SGLT-2 inhibitors approved for type 2 diabetes treatment by the U.S. Food and Drug Administration: canagliflozin, dapagliflozin, empagliflozin, and ipragliflozin. You can take a printed version of this list to your doctor's office to make an informed decision.
SGLT-2 inhibitors reduce blood glucose levels
SGLT-2 inhibitors are an important component of diabetes treatment for many reasons. In addition to lowering blood glucose levels, these drugs also reduce insulin and GLP-1 receptor agonist levels. These medications work to boost the production of ketone bodies, which are more efficient substrates for myocardial energy generation. This results in improved cardiac efficiency and contractility. This class of drugs also helps control blood pressure. A recent meta-analysis of four large randomized trials found that combination therapy patients lost more weight than patients treated with monotherapy. Additionally, combination therapy patients had significantly lower systolic blood pressure and hemoglobin A1c levels than patients treated with monotherapy.
Despite their popularity, SGLT-2 inhibitors have their own risks. Some of these drugs have been associated with increased risks of amputations. Another serious side effect is diabetic ketoacidosis, a potentially fatal and life-threatening condition. Despite these risks, SGLT2 inhibitors are generally safe for use in the treatment of type 2 diabetes. They may not be a good choice for those with severe kidney disease or a history of DKA.
In addition to lowering blood glucose levels, SGLT2 inhibitors have an added benefit: they have good kidney protective effects. This means that they can delay the development of diabetic nephropathy. As a result, SGLT2i are a promising type of diabetes treatment. This treatment option is worth exploring further. You can learn more about it below. And remember, a good diabetes treatment regimen is one that is safe and effective for your body.
SGLT-2 inhibitors improve glycaemic control
A recent study showed that SGLT-2 inhibitors improve gastrointestinal symptoms and glycaemic control in type II diabetic patients. These agents block a protein called sodium-glucose cotransporter-2 (SGLT2) that helps regulate glucose levels. The results suggest that these drugs improve glycaemic control and improve CV and renal function.
The authors of the study found that the SGLT-2 inhibitors improved glucose control in patients with type 2 diabetes, and decreased glycosylated hemoglobin A1c and fasting plasma glucose levels. They also reported reduced body weight and reduced insulin dosage. Further, they found that SGLT-2 inhibitors improve glycaemic control in patients resistant to metformin.
A stepwise dose-reduction strategy of insulin is recommended rather than total discontinuation because it may cause hypoglycemia and DKA. Similarly, antiglycemic agents should not be adjusted in patients who exceed their glycemic targets and those who experience frequent hypoglycemia. However, patients should be informed about the risk of hypoglycemia with all antiglycemic agents, including SGLT-2 inhibitors.
The SGLT-2 inhibitors were not without side effects. A recent study in Type II diabetic patients showed that SGLT-2 inhibitors improved glycaemic control in a majority of patients. However, the adverse effects associated with SGLT-2 inhibitors are rare and usually confined to the first year of treatment. The researchers recommend caution and cautious use of these agents.